Pill perfection: Choosing the right pill for you
Let us demystify all the latest pill options so you can find one that fits.

So you’ve thought about all of your birth control options and decided the pill is the right method for you. Or maybe you’re already using the pill, but you’re annoyed with one of the side effects and want to switch to a different type. So…which pill would be best?
There’s a huge range of pills to pick from: some claim to help reduce acne, others boast lessening PMS symptoms, a few have cute cases, and they all have odd names.
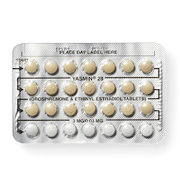
First, the good news: while only three types of pills have been specifically studied and marketed for improving acne, all of them likely help with smooth skin. More good news: all pills will also make your period lighter and less painful. Still more good news: there’s evidence that Yaz, Yasmin, and many of the other pills will also help with really intense PMS symptoms.
There are actually only two basic types of pill:
Progestin-Only Pills (aka the mini pill or POPs)
The progestin only pill isn’t as effective as the combined pill, so it’s usually recommended when women can’t take estrogen. This isn’t common, but could affect you if you have migraines with visual effects, really high blood pressure, or a blood clotting problem. Since most young women aren’t in these categories, we’ll focus on the other type.
Combined Pills (aka combined oral contraceptives or COCs)
The combined pill has both estrogen and progestin and, when taken correctly, is super-effective at preventing pregnancy. Your body makes estrogen and progestin naturally, and, compared to the pills of the 1970s, all pills on the market today have low doses of these hormones.
Phases and Cycles and Brands, Oh My!
The combined pill delivers hormones in one of two ways: monophasic, or multiphasic.
Monophasic pills have constant levels of hormone in them for the whole month. They tend to decrease the chance of spotting in between periods, especially if you choose to skip the placebo pills and, as a result, skip your period. If you’re interested in having fewer periods, talk with your nurse or doctor about a monophasic, extended cycle pill.
Multiphasic pills have varying levels of hormones in them throughout the month; they’re designed to mimic the normal hormonal changes in your menstrual cycle.
There are also a variety of cycle lengths available. Some combined pills have 21 days of active pills and 7 days of placebo pills, others have 24 active and 4 placebo pills. The fewer placebo pills there are, the shorter your period will be. The newest pills are designed to be used continuously for three months, so you have only 4 periods a year.
But if your budget is tight, you don’t have to buy extended-use brands to have fewer periods; you can use any kind of pill continuously, just by skipping the placebo pills. Monophasic pills used continuously will cause less breakthrough bleeding. In general, the most affordable pills out there are ones that have been around for a while and have generic versions—all generics are 21 active and 7 placebo. The newest, patented pills have big advertising budgets, but may not work any better for you than a generic pill.
Getting to Know You…
It’s going to take your body a few months to get used to any form of hormonal birth control. You have to have the patience to get through the first few months to know exactly how a new pill will work for you. All pills may cause spotting, especially in the first months. Remembering to take your pill every day at the same time will help your body adjust faster. If you have problems with spotting, bloating, mood changes or other issues for more than the first few months, let your doctor know. You may want to try a different pill—for example, switching to a pill with a different type of progestin in it might alleviate some or all of your side effects. Of course, when you switch you’ll have to start the adjustment period all over again!
Remember, the pill won’t protect against sexually transmitted infections, and it has to be taken just as your doctor directs to work best. So talk to your nurse or doctor and weigh the evidence against the advertisements!
How do you feel about this article?

Heat up your weekends with our best sex tips and so much more.