Will over-the-counter birth control pills ever happen?
There’s been lots of talk, but when will we actually be able to get birth control pills without a prescription?

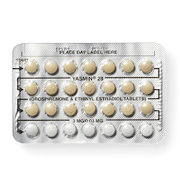
In recent years there have been plenty of headlines about the birth control pill becoming available over the counter. There has even been a proposal about it in Congress. But what does all of this actually mean for women who use the pill?
First, a definition.
What exactly does “over the counter” mean, anyway? It makes it sound like you’ll be handed the product over a counter, right? Like maybe there will be a discussion with a pharmacist or a clerk involved, because they’re keeping the product you want behind said counter and you’ll need their help to get it. What it actually means is that a product is in the aisles of the store and you can buy it whenever you want—no conversation needed. Aspirin, condoms, and levonorgestrel emergency contraception are all sold this way.
So… when can I get my birth control pills over the counter?
Right now, there aren’t any states where buying a pack of birth control pills is as simple as buying aspirin, but there are a few where you don’t need to visit a doctor or nurse practitioner for a prescription.
On January 1, 2016, an Oregon law went into effect allowing women ages 18 and older to get a prescription directly from a pharmacist for birth control pills and patches. On April 8, 2016, California put a similar law into effect, allowing pharmacists to prescribe the pill, the patch, the ring, and the shot to women of any age. The thing to note is that these methods are actually behind the counter—women have to consult with a pharmacist to get them.
Law makers in Hawaii, Missouri, South Carolina, Tennessee, Washington state, and Iowa are catching on and considering laws allowing pharmacy access for birth control pills.
What are the pros and cons of getting birth control pills over the counter?
Put simply, the biggest benefit is the time you can save not having to visit a health care provider for a prescription. If you are low on pills, it will be a lot faster to go straight to the pharmacy rather than have to make an appointment or wait at the clinic. Saving this time and money is a big deal for lots of people: one study found that almost a third of women seeking hormonal contraception had trouble either obtaining or filling their prescription.
If someday methods of birth control that are currently prescription-only—like the pill, patch, ring, and shot—do become available truly over the counter, there may be drawback for folks with health insurance. Getting any medication over the counter may mean that it’s not covered by insurance. The Affordable Care Act requires that most insurance plans cover contraception without co-pays, but some plans may require a prescription to trigger that coverage.
Is it safe to ditch the prescription?
Turns out women are pretty good at figuring out if they need birth control. They’re also good at figuring out if they have a medical condition that may make birth control pills unsafe. Birth control pills are not addictive, nor can you overdose on them, and those are the Food and Drug Administration’s main concerns when they require a drug to be given only by prescription.
The U.S. wouldn’t be the first place to let women get birth control pills without seeing a health care provider. In fact, in most countries women can get birth controls pills without a prescription.
Will there be true in-the-aisles access in the U.S. someday?
There’s a team of people working on making this a reality. Experts think that a progestin-only or mini-pill will likely be the first pill available in the aisles. Since birth control pills are safe and sold this way in many countries, seems like it’s only a matter of time before the U.S. catches up.
How do you feel about this article?

Heat up your weekends with our best sex tips and so much more.